Hepatitis C is a liver infection caused by the hepatitis C virus (HCV). Hepatitis C is spread through contact with blood from an infected person. Today, most people become infected with the hepatitis C virus by sharing needles or other equipment used to prepare and inject drugs. For some people, hepatitis C is a short-term illness, but for more than half of people who become infected with the hepatitis C virus, it becomes a long-term, chronic infection. Chronic hepatitis C can result in serious, even life-threatening health problems like cirrhosis and liver cancer. People with chronic hepatitis C can often have no symptoms and don’t feel sick. When symptoms appear, they often are a sign of advanced liver disease. There is no vaccine for hepatitis C. The best way to prevent hepatitis C is by avoiding behaviors that can spread the disease, especially injecting drugs. Getting tested for hepatitis C is important, because treatments can cure most people with hepatitis C in 8 to 12 weeks.
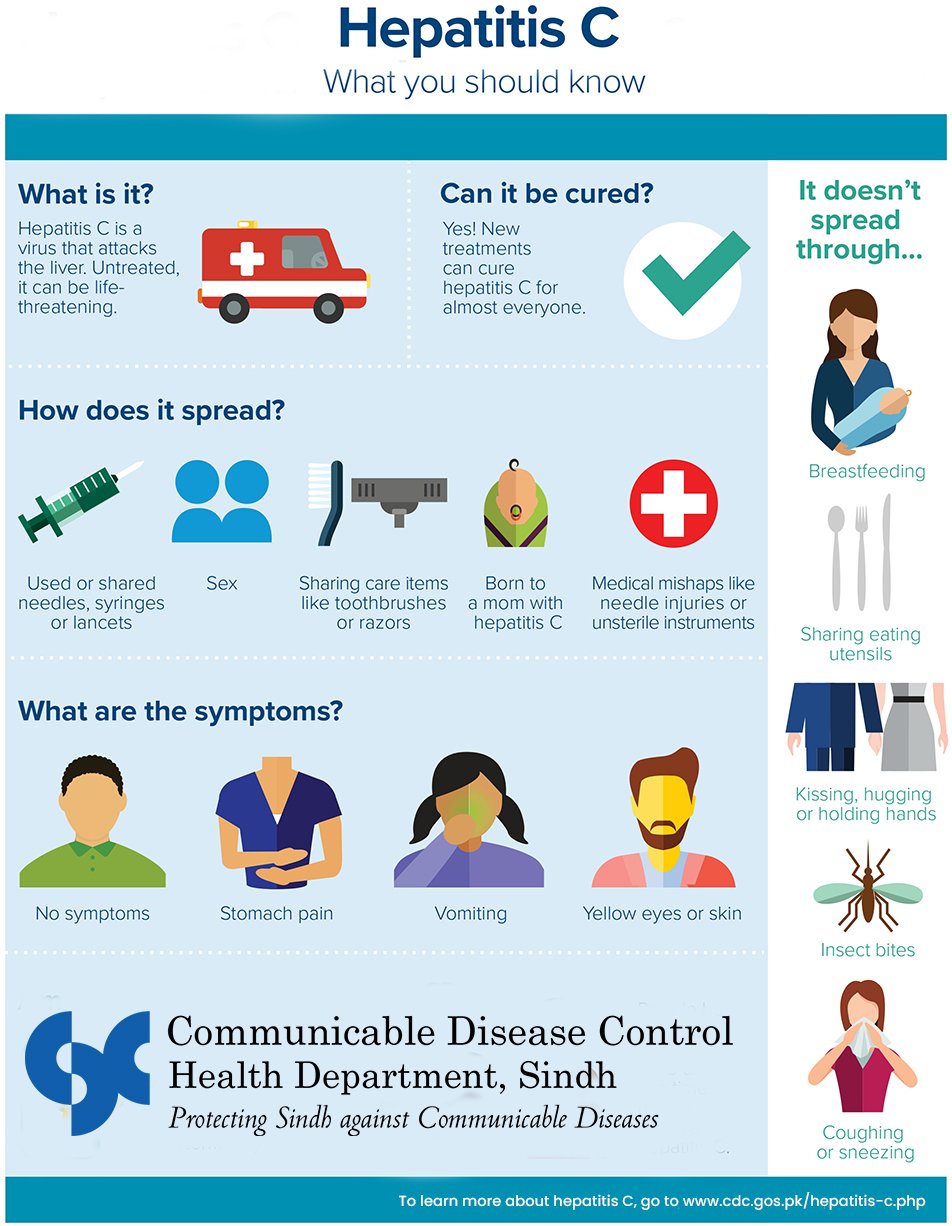
HCV is transmitted primarily through parenteral exposures to infectious blood or body fluids that contain blood. Possible exposures include:
Although less frequent, HCV can also be spread through:
Many people newly infected with the hepatitis C virus don’t have symptoms, don’t look or feel sick, and therefore don’t know they are infected. For people who develop symptoms, they usually happen 2–12 weeks after exposure to the hepatitis C virus and can include yellow skin or eyes, not wanting to eat, upset stomach, throwing up, stomach pain, fever, dark urine, light-colored stool, joint pain, and feeling tired.
Most people with chronic hepatitis C don’t have any symptoms or have only general symptoms like chronic fatigue and depression. Many people eventually develop chronic liver disease, which can range from mild to severe and include cirrhosis (scarring of the liver) and liver cancer. Chronic liver disease in people with hepatitis C usually happens slowly, without any signs or symptoms, over several decades. Chronic hepatitis C virus infection is often not recognized until people are screened for blood donation or from an abnormal blood test found during a routine doctor’s visit.
You should get tested for hepatitis C if you:
Treatment is recommended for all people, including non-pregnant women, with acute or chronic hepatitis C (including children aged ≥3 years and adolescents). Current treatments usually involve just 8–12 weeks of oral therapy (pills) and cure over 90% with few side effects.
People with chronic hepatitis C and those with cirrhosis (even if they have been cured of their hepatitis C infection) should be monitored regularly by a doctor, because these people have a continued risk of complications of advanced liver disease, including liver cancer. In addition, people living with hepatitis C should: